Bonjour Docteur!/ Hi Doc!
Experts discuss the vaccine topic
CoronaSTAVELOT.com
Thanks for visiting!
To translate this page, select your
language from the dropdown menu below:
Servez-vous du traducteur ci-dessus si besoin.
This panel discussion was published at this link.
From MedScape - General Surgery
COVID Positive After Two Vaccine Doses?
What It Means
Robert D. Glatter, MD; Peter M. Antevy, MD; Angela L. Rasmussen, MA, MPhil, PhD; Nicole M. Iovine, MD, PhD
March 09, 2021
Robert D. Glatter, MD: Hi and welcome.
I'm Dr Robert Glatter, medical advisor for Medscape Emergency Medicine.
Although you may be certain that you received the COVID-19 vaccine, you can still test positive for COVID-19 after receiving one or even two doses of the vaccine.
Here to discuss this is a distinguished panel of experts:
Dr Peter Antevy, a pediatric emergency physician and EMS medical director for Coral Springs Parkland Fire Department in Coral Springs, Florida;
Dr Nicole Iovine, an infectious disease physician and epidemiologist from the University of Florida; and
Dr Angela Rasmussen, a virologist with the Center for Global Health Science and Security at Georgetown University.
Welcome, everyone. Thanks so much for joining me.
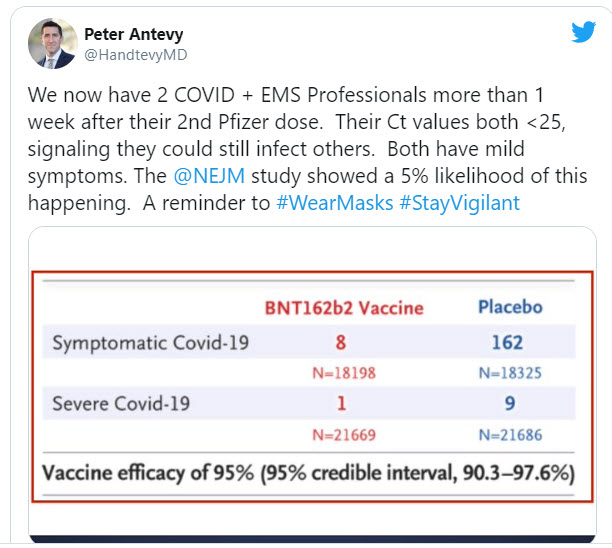
It says that we now have two COVID-positive EMS professionals more than 1 week after their second Pfizer dose. Their Ct values are both less than 25, signaling that they could still infect others. Both have mild symptoms at this time. The New England Journal of Medicine study showed a 5% likelihood of this happening, a reminder to #WearMasks and #StayVigilant.
Antevy: I was really surprised at this. We had a hard time getting our folks in the EMS world vaccinated to begin with. Once they got vaccinated, we all took a deep sigh of relief and felt good about it.
One of the paramedics had COVID in November with GI symptoms, a headache, and nausea. She then got vaccinated in January, and a week after her second dose, she had a sinus infection. Before the ENT would see her, he
said, "You have to get tested." She tested PCR positive. Interestingly, she lives with her sister and spent time with her brother-in-law, neither of whom got infected. That gave us a little bit of information.
Aside from the EMS professional, let me tell you about another case that just happened. A chef at an assisted living facility was vaccinated, and 4 days after his second vaccination, his wife gets COVID and brings it home. He is now symptomatic and cooking food for a lot of people. Needless to say, the food was thrown away and he was sent home. He's doing well.
My question to the experts on the call is, will these people transmit to others? We have the policy of 24-hour masking at the fire stations and we're pretty solid about that.
Glatter: This is really a concern of transmission and everyone is fearful of this. I want to just back up and have the group talk about reasons for testing positive between doses or after vaccination. Angie, can you give a few reasons why people are testing positive and what could be happening?
Rasmussen: People are testing positive because they're getting infected. That doesn't necessarily mean that they are contagious or shedding infectious virus, but people are not going to test positive based on the vaccination itself. All the diagnostic tests, as far as I'm aware, don't exclusively target the spike protein. That's what the vaccines encode.
If anybody tests positive shortly after vaccination, it's because they either are infected or they have recently been infected. We also know that once people recover from COVID-19, they can shed RNA from their infection for a period of weeks. It means that they were infected recently or at some point in the very near past. What it doesn't mean is that they are necessarily going to be transmitting virus or that they are, in fact, contagious.
Glatter: We don't know that for a fact. That's the question we're after right now with the studies that are ongoing. Certainly, between doses we know that we're partially covered — they say 50% after the 14th day, give or take — but that's still not enough. Obviously, if you were exposed at some point in the window of opportunity where you could get the virus, you're going to test positive.
Now, do you continue getting vaccinated once you've tested positive? That's an important question, because I've had many people say, "I shouldn't get the vaccine or the second dose," and others are saying, "When I feel better and get better, I should."
Nicole, do you want to weigh in on that?
Iovine: I would start by tagging onto the prior conversation that immunity develops along a temporal spectrum. There's nothing magical about it at 14 days, like a switch that turns on and now you're immune. The fact that people can be infected at points in time after getting the first or the second vaccine is really not surprising.
For people who develop COVID between the vaccines or who recently had COVID, I always tell them that they still need to get vaccinated because the vaccine is going to give them a targeted response against the part of the protein that we know is important for infection.
By getting the vaccine, you're going to develop neutralizing antibody as opposed to this broader response, which sounds like a good thing. Many of the antibodies that you get from natural infection are not protective against a second infection. I always encourage people, regardless of their COVID history, to still get the vaccine when they are eligible for it.
Glatter: That provides the rationale for getting vaccinated even if you've had the infection, because it's very specific to the spike protein. People often give me the argument that "I've had the infection. I don't need the vaccine." I think that's a very important point to take away from that.
Rasmussen: If I could just add to that very quickly that several studies have now been done showing that people who were seropositive for COVID, who had prior infections, see huge increases in their levels of neutralizing antibodies after a single dose of the vaccine. Vaccination can act as a booster for the immunity that is produced by a natural infection.
Antevy: I have one other question for you guys on that one. I have a medic
who got vaccinated, got COVID after the first dose, and now someone from the Department of Health is asking him to repeat the full double-shot series. I disagreed with that. Am I correct?
Iovine: No, that's not what the CDC recommends. They recommend that you just complete the series of two shots.
Glatter: My concern is that the variants are going to have an effect on vaccination. Some people are reluctant and want to wait and get the next round of vaccine. I think that's just incorrect reasoning. I'd like to have the group weigh in on this. Angie, if you want to start.
Rasmussen: Yeah, that's also incorrect reasoning. Even in the variant that was first detected in South Africa (the B.1.351 variant), that seems to be at least partially capable of evading some of the immunity produced by vaccination; it was still efficacious. It still protected people from severe disease. It may not be at the same levels as the protection against the previously circulating variants (or the variants that are actually still circulating) throughout most of the world. But it still does offer significant protection, especially against the endpoints that we most want to avoid, specifically severe disease and death.
That's the important message that I'm trying to get out. The vaccines still work. We may need boosters in the future, and I'm glad that all of the vaccine manufacturers are developing them now rather than waiting until they're absolutely necessary. But that shouldn't deter people from getting the vaccine now. Personally, as soon as the vaccine becomes available to me, I will be getting it regardless of which variants are circulating in my community.
Iovine: That's a very important point because the vaccine efficacy only refers to the reduction in getting infected. It does not give you any information on the severity of disease, if you do get it, or on mortality.
We know this from influenza vaccination. Influenza vaccine efficacy is never more than 50%, maybe 60%. But we know that it is hugely beneficial because it prevents hospitalizations and it prevents mortality across the board in many different patient groups. This is true also of the COVID vaccine and the variants; it still has all of these tremendous beneficial effects that Dr Rasmussen is reporting. We shouldn't get stuck on a number on vaccine efficacy because there's so much more to the protection that a vaccine offers.
Glatter: To your point, Nicole, if we look at the Israeli experience so far, that's sort of a real-world experiment of what the Pfizer vaccine can do. Over 500,000 have been vaccinated with two doses. Only 544 people caught the virus 7 or more days after getting their second dose of the vaccine, so 93% percent effectiveness. There were no deaths and four severe cases among 500,000 or so vaccinated. There were 15 hospitalized and four did have severe illness. But again, no one died.
Antevy: This is something that I heard from Dr [Michael] Osterholm this morning (I listened to his podcast). He thinks that because the UK variant is already on our shores — and he believes it is going to be tremendously greater in the March timeframe — perhaps we vaccinate at least as many as we can of our seniors with one dose. Forget about the second dose for now, because we have up to 6 weeks to get it.
I would love to hear what Nicole and Angie think about this. Is it time for us to change our strategy to first get vaccines out into the population to prevent what's coming a month from now?
Iovine: This discussion has been going on even before the variants came out. Is it better to give a single vaccine to bigger numbers of people rather than fully vaccinating a smaller group? The logic to giving a single dose of vaccine to more people is that it will reduce infections. You are just trying to make it harder for the vaccine to find a susceptible host. The other benefit to that approach is that it's also harder for it to mutate again into something perhaps worse. That's the logic behind that approach.
There are arguments both ways, so it's pretty difficult to know. Honestly, the vaccine response is more fraught with supply of vaccine and the distribution. I don't think we're at a point right now where we can easily choose one or the other, because we're still just trying to get even a single shot out to people. I don't know, Angie, if you have another point of view.
Rasmussen: I'm about to make the "against" argument. I agree with Michael Osterholm on a lot of things, but not on this one, for a couple of reasons — some are scientific, some having to do with practical and logistical concerns, and some of them having to do with vaccine competence over the long term.
The scientific reason is that this has been tested only out to 6 weeks, and there seem to be more neutralizing antibodies induced that are more likely to be protective. Now, granted, we don't have really good correlates of protection, but neutralizing antibodies are probably very important for vaccine protection. Those are really induced at the highest levels after the second dose. I'm concerned about extending that interval between doses longer than 6 weeks, because it might mean that people would actually have diminishing protection beyond the 50% that has been looked at based on the clinical trials.
In terms of distribution, I completely agree with Nicole that part of this is a supply-and-distribution issue. I would be all for putting as many shots in as many arms as we can if we could guarantee that we were going to have those second shots for those people within that 6-week time frame.
Then the third reason is, if the worst-case scenario happens and people thought that they were more protected when they weren't after a single shot longer than 6 weeks, that's going to discourage people from taking vaccines over the long run. We don't want to be decreasing confidence in these vaccines because they've actually exceeded our wildest expectations about efficacy. I think that it's really important to communicate with people who are vaccine hesitant because the process has been expedited that we didn't cut corners. Many people are going to be saying, "Well, if we went through all these phase 3 clinical trials and you're telling me that this is safe, why are you now tinkering with the dosing recommendations?"
For all those reasons, I think it's really important to vaccinate as many people as possible. But ultimately, even if we did that, we still wouldn't have enough vaccine to protect all of the most vulnerable people. Instead, we should be urging people to double down on the nonpharmaceutical interventions that we know also reduce community transmission: masking, social distancing, staying home if you can, avoiding gatherings and enclosed spaces, ventilating if possible, washing your hands, and disinfecting high-touch surfaces.
Glatter: I totally agree with you, Angie. Interestingly, with the AstraZeneca vaccine — you may have seen the data and there were multiple trials within this study — they found that the first shot, on average, conferred 76% protection against symptomatic infections from 3 weeks until 90 days, and by their data, reduced transmission by about 67%, arguing for this 12-week delay that the UK now is saying that they are doing. To that point, certainly a 12-week delay is not a longer-term delay that we're looking at necessarily, but there is some evidence that we could probably get away with it.
Rasmussen: Yes, for the AstraZeneca vaccine (and other viral vector vaccines), but the mRNA vaccines are a completely different vaccine technology.
One of the advantages of using a viral vector vaccine — and this is probably why Johnson & Johnson is having more luck with a one-shot regimen with their viral vector vaccine — is that these are viruses that are actually going through part of the replication cycle. They're ringing a lot of the alarm bells of the innate immune system, and they're more likely to induce a robust immune response after a single dose rather than the mRNA vaccines, which basically express the spike protein. They probably do trigger some of those innate immune system alarms because they're exogenous RNA coming in from outside the cell, but not to the same level that a replicating or partially replicating adenovirus would. There are data to support a 12-week interval for the AstraZeneca vaccine, but there are no data to support that for the Pfizer or Moderna vaccines.
Antevy: Speaking of data, I'm actually almost done with a trial. I'm doing an antibody study on 80 people. They range in age from 20 to over 100 years old. We're doing antibody testing on days 0, 14, 21, and the next will be day 28. I have my data up in front of me. You can't see it, but there is a very clear distinction that as they get older (every decade), we see a gradual reduction.
Remember, this is a qualitative antibody test or rapid, but only 18% of the 91- to 100-year-olds showed any antibody formation on day 21, whereas the 20- to 50-year-olds all showed antibody development. The older population that we're trying to protect does perhaps need that booster sooner as opposed to a younger person who maybe has a more robust immune system.
On day 28, we're going to be testing for neutralizing antibodies as well. It'll be interesting to see what data we get.
Glatter: That's pretty impressive. Any thoughts on that, Angie?
Rasmussen: Those are really interesting results. They're also concerning, given that that is one of the groups that is the most vulnerable and most in need of protection. It is also concerning that they are not benefiting at all from the first shot, at least in terms of their antibody responses. It will be interesting, though, to see how many neutralizing antibodies they have mounted. I'm assuming that's a more quantitative test anyway. That may be less worrisome once you see the neutralizing antibody data. But that certainly argues against just doing one shot in vulnerable groups based on age.
Iovine: Your finding also fits with a widely held and broad idea of immune senescence — that as we become older, our immune system mounts a less robust response. In fact, that is the reason why, for the flu vaccine (a more familiar vaccine), we have a high-dose antigen flu vaccine for older people. I believe that's also true for the shingles vaccine; I think that the Shingrix vaccine had the higher antigen components than what the Zostavax had. That is disappointing, but it's not entirely surprising what you're seeing.
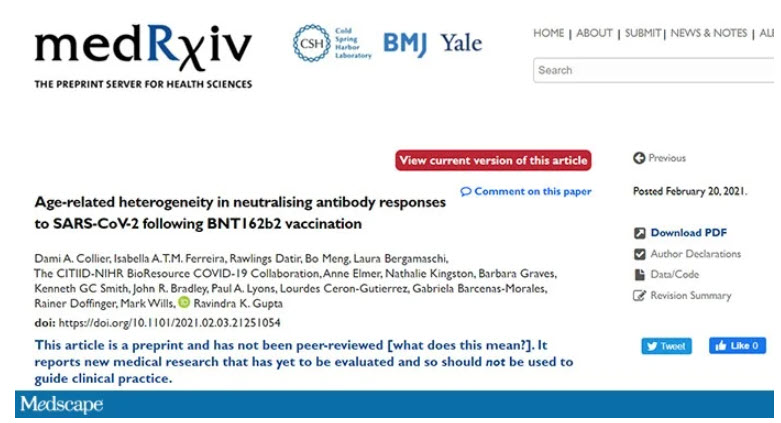
Antevy: There was a paper that was just published on medRxiv on neutralizing antibody responses. It seems to be that of those under 80 years of age, 11 of 11 developed neutralizing antibodies and then over 80 years of age, only 50% developed neutralizing antibodies. This study out of the UK showed similar findings to my study. I think we do have to think about that population a little bit more specifically.
Glatter: This is really interesting. It brings me to the idea of these adenovirus vector vaccines, which we just touched on earlier. Looking at the Sputnik V vaccine and the concept of a heterologous prime boost, Angie, I was hoping you could get into that because the amount of immunity we get with that technique seems to be promising. Is that your take on this?
Rasmussen: For adenovirus vaccines, a heterologous prime-boost regimen is probably the way to go, because there always is the possibility of generating vector immunity that can make a booster dose from the same adenovirus as the prime less effective, because you're effectively going to have antibodies against the vaccine itself rather than the antigen that you're trying to immunize with.
The way adenovirus vaccines work is that you have to be infected with the adenovirus and then it will start expressing the antigen. There are other types of viral vector vaccines that are essentially pseudotyped viruses that don't have to actually do that. The Ebola vaccine is a good example of that; it's an rVSV vector vaccine.
But the adenovirus vaccines are susceptible to antibodies against adenoviruses. And so, if they can't infect the cell because you have antibodies against the vaccine, then they're not going to be expressing the antigen and you won't get that boost. A heterologous regimen for those is great. I think that going forward, especially if we're in a situation where these variants emerge that are reducing the overall protective efficacy of some of these vaccines, we may have to start doing heterologous boosting over time.
I'm assuming that you probably can't come back with the same adenovirus vector over and over again and give people a boost. You might be looking at heterologous boosting regimens across vaccine platforms, where you would get your first vaccine with the Johnson & Johnson and then later you would get a booster with an mRNA vaccine or a protein subunit vaccine, something like that. I think that is going to allow us to be as flexible as possible with emerging variants going forward.
We should start looking at different heterologous boosting regimens now because none of us (in the United States or North America) are going to be getting access to the Sputnik V vaccine unless we go to Russia or Brazil. We should be thinking about heterologous boosting regimens in general.
Glatter: In order to get to herd immunity, do you see any specific combination as more valuable than any other, looking at where we are right now, sort of on the trajectory?
Rasmussen: That's a really good question. A lot is going to depend on the vaccine rollout globally, especially in lower middle-income countries where there might not be as strict of a cold chain. You're going to see a much bigger use for the adenovirus vector vaccines, as well as the protein subunit vaccine, such as what's made by Novavax, because there aren't those really stringent ultra–cold chain requirements as for the mRNA vaccines.
As we start to roll the vaccine out globally — which we should have been thinking about prior to this — it's going to take several years to immunize the globe. I think that these various vaccine technologies are going to be different, potentially in different combinations in different parts of the world, depending on what is easiest to distribute and roll out to those populations.
Glatter: I want to ask the group for some pearls to wrap up here. Peter, if you could give us a few takeaways from our discussion.
Antevy: My biggest push at this time is to get as many people vaccinated as possible, even if we have to stretch out and use our supply for those first doses. The national effort will hopefully provide us with more vaccines because my sites are only getting 50 doses a day and I can do 1000 a day. I'm hoping for that and I hope that people continue to do the right things (eg, wear masks) moving forward.
Iovine: I would say that when people ask which vaccine should I get, I would say the vaccine that is available to you is the one that you should get. Do not delay.
Rasmussen: As a final thought, I'd like to agree with what both Peter and Nicole said, especially getting whatever vaccine you can as soon as you can. But in the meantime, also take precautions, because I think a lot of people have been thinking about the question of whether vaccines can prevent transmission, whether they can protect against infection, and feeling like, Is this going to go on forever? Are we going to be living like this for the foreseeable future into 2022, 2023, and beyond?
The answer is no, especially if everybody is getting vaccinated, and until everybody gets vaccinated, if everybody is really doubling down on the precautions to reduce community transmission. We don't actually have to hit the herd immunity threshold to start relaxing some of these restrictions if we can get community transmission low enough.
Glatter: Thank you. This has been so informative and an important discussion around this very critical topic.
Robert D. Glatter, MD, is an attending physician at Lenox Hill Hospital in New York City and assistant professor of emergency medicine at Zucker School of Medicine at Hofstra/Northwell in Hempstead, New York. He is an editorial advisor and hosts the Hot Topics in EM series on Medscape. He is also a medical contributor for Forbes.
Peter M. Antevy, MD, is an EMS physician and medical director for Coral Springs–Parkland Fire Department in Florida. He is a member of the EMS World editorial advisory board.
Angela L. Rasmussen, MA, MPhil, PhD, has studied a variety of viruses, including Ebola, using systems biology and genomics to examine the virus and host responses. In the current pandemic, she's used Twitter to counter misinformation and misinterpretation of data.
Nicole M. Iovine, MD, PhD, is an infectious disease specialist at the University of Florida College of Medicine, Division of Infectious Diseases and Global Medicine, in Gainesville, Florida. Her research expertise includes the clinical manifestations, epidemiology, and genetics of influenza viruses, with a focus on understanding the innate defenses against and best treatment options for multidrug-resistant Gram-negative infections and similar diseases.
Nasopharyngeal swabbing for SARS-CoV-2 samples
A how to video.
Don't try this at home ...
"Didn't hurt a bit ... (but I was wearing my lucky purple gloves)."
-----------
Our view of the world's COVID-19 challenge this day April 17 (in English) >>>>>>>>>>
Same view of the world situation but en français >>>>>>>
Les données pour Belgique, hier le 16 avril >>>>>
And finally, yesterday in Belgium, in English >>>>>
Testing for COVID-19 as seen in the world
Take a second to look at this little video.
Then try to explain why the results are as shown.
Clearly, not everyone is on the same wavelength.
The Youtube link if needed: https://youtu.be/Nfgds2annDw
Fitting today's results of testing locally here in Belgium with these findings, is not easily done.
Is "find them fast" before they "get really sick" : "early detection/ early treatment," what we're seeing in these results?
How can outcomes so far observed from testing during this pandemic, help define the right balance?
As we group together to try and interpret these various and often confusing results of laboratory tests, let's not forget the most useful thing to do :
When all else fails, let's examine the patient.
Not everybody is up for that : "What?! Examine the patient and catch the virus?! No thanks!"
23 March, 2020 : I have added an update to this article. While primarily concerned with the Netherlands' new approach to managing COVID-19, this newer article also contains some interesting data related to world practices for testing for the virus, and related to outcomes. Have a look.
Sharing Clinical Information (Partager)
E:
(en français ci-dessous)
COVID-19 ...
Most won't get it. They will be anxious. That's an opportunity for therapeutic intervention.
Some will get it and be asymptomatic or mildly ill. That may require some therapy, even if presenting few challenges.
Some will get it and be severely ill with COVID-19 (positive test, pneumonia, thick tenacious pulmonary secretions, increased work of breathing, hypoxia, hypoxemia, and need for supplemental oxygen, mechanical ventilation and ICU care).
That speaks to the need for the best therapy, to save a life.
No matter the care offered, some (3.44% is my number today), will die.
It is that thought, that existential nuissance resurfacing in the minds of all, that has everybody scared.
Not: "Are we gonna run out of Cheerios?!"
The Dalai Lahma, I am told, spends several hours each day, in meditating on his own personal death. Most people, aren't into that.
Two evenings ago, I was listening to a Chinese physician speak about his personal and professional experiences in Wuhan since end of January. He is a clinician seeing patients, Director of several Respiratory and Critical Care Services, a Researcher, and clearly, judging from his actions taken in support of very sick patients, quite compassionate. How I heard him speak to patients, was part of healing them. I listened 40 minutes to him speak (in mostly very good English, and certainly better than my Cantonese), about what he had learned. He learned many things in a short time. A February cram course.
And as he spoke, certain things caught my attention as a physician. I several times found myself thinking: "That information should be shared globally," and taking note.
So this article, and those that may follow, are intended to do just that. In a small way of course. But perhaps, if it helps to better care for 1 patient, sharing information will have been effective, and worth the small effort here.
I welcome non-medical readers as well here.
But bear in mind, that this will and should at times, become quite technical. But there is nothing here to hide. If a certain need for more intensive therapy develops, speak to your physician if he hasn't yet seen certain new perspectives. These have now begun coming out of China. The most useful information that catches my attention, will be repeated here, and with appropriate medical reference articles when available.
This is not offered as a diagnosis or suggestion for treatment of your cold, if you have one. It is offered as a source of potentially useful information for those who now must do just that: diagnose and treat patients with COVID-19.
My personal and professional experience with COVID-19 is zero. With luck it will stay that way.
The majority of physicians who will be called upon to address COVID-19 diagnosis and therapy are in the same boat: experience = 0. But like it or not, they will be in the driver's seat.
And at that point, the patient is no longer the only one anxious in the exam room.
F :
COVID-19 ...
- La plupart des gens ne seront pas contaminé avec ce virus. Ils seront inquiets. Cette inquiétude est une opportunité d'intervention thérapeutique.
- Certains l'obtiendront se virus, et seront asymptomatiques ou légèrement malades. Cela peut nécessiter une thérapie, même si elle présente peu de défis.
- Certains l'obtiendront et seront gravement malades avec COVID-19 (test positif, pneumonie, sécrétions pulmonaires tenaces épaisses, augmentation du travail respiratoire, hypoxie, hypoxémie et besoin d'oxygène supplémentaire, de ventilation mécanique et de soins intensifs).
Cela témoigne de la nécessité de la meilleure thérapie, pour sauver une ou plusieurs vies. - Peu importe les soins offerts, certains (3,44% aujourd'hui est mon chiffre) mourront. C'est cette pensée, cette nuissance existentielle refaisant surface dans l'esprit de tous, qui fait maintenant peur à tout le monde. Ce n'est pas la pensée qu'ils pourraient manquer de dosettes de café pour leur Senseo. Le Dalaï Lahma, me dit-on, passe plusieurs heures par jour à méditer sur sa mort personnelle. La plupart des gens ne vont pas faire de même.
Il y a deux soirs, j'écoutais un médecin chinois parler de ses expériences personnelles et professionnelles à Wuhan depuis fin janvier. C'est un clinicien qui voit des patients, directeur de plusieurs services de soins respiratoires et intensifs, un chercheur publié, et clairement, à en juger par ses actions prises en faveur de ses patients très malades, un modèle de compassion. La façon dont je l'entendait parler à ses patients faisait partie de leur guérison.
Je l'ai écouté 40 minutes parler (dans un assez bon anglais, et certainement mieux que mon Cantonais), de ce qu'il avait appris de ses expérience tous le long du mois de février.
Et pendant qu'il parlait, certaines choses ont attiré mon attention: Mon attention de médecin.
Plusieurs fois, je me suis retrouvé à penser: «Ces informations devraient être partagées à l'échelle mondiale» et j'en ai pris note.
Donc, cet article, et ceux qui peuvent suivre, sont destinés à faire exactement cela.
D'une petite manière bien sûr.
Mais peut-être que si cela aide à mieux soigner 1 patient, le partage d'informations aura été efficace, et cela en aura valu l'effort minime ici.
Je souhaite également la bienvenue aux lecteurs non médicalisés.
Mais gardez à l'esprit que cela deviendra, et devrait parfois devenir, assez technique.
Mais il n'y a rien ici à cacher.
Si un certain besoin de thérapie plus intensive ou utile se développe, parlez-en à votre médecin s'il n'a pas encore vu certaines nouvelles perspectives, certaines astuces efficaces. Celles-ci ont maintenant commencé à sortir de la Chine. Les nouvelles thérapies prennent un peu de temps pour être intégrées dans la pratique de tout médecin, qui est normal et prudent.
Les informations les plus utiles qui attirent mon attention seront répétées ici et avec les articles de référence médicaux appropriés, joints lorsqu'ils seront disponibles.
Ceci n'est pas offert comme diagnostic ou suggestion pour le traitement de votre rhume, si vous en avez un.
Ni pour aucune autre maladie, y compris COVID-19.
Il est proposé comme une source d'informations potentiellement utiles pour ceux qui doivent désormais faire exactement cela: diagnostiquer et traiter les patients atteints de COVID-19.
Mon expérience personnelle avec COVID-19 est nulle: 0 en chiffre. Avec de la chance, cela restera ainsi.
La majorité des médecins qui seront appelés à aborder le diagnostic et la thérapie au COVID-19 sont dans le même bateau: expérience avec = 0. Mais que cela vous plaise ou leur plaise ou non, ils seront aux commandes.
Et à ce moment-là, ce n'est plus le patient qui est le seul inquiet dans la salle d'examen.